Whiplash is a common neck injury that often happens in car accidents when the head is suddenly jerked back and forth, straining the neck’s soft tissues. This rapid “whipping” motion can overstretch muscles, ligaments, and joints in the neck and upper back, leading to pain and stiffness. If you’re reading this after a crash or injury, you’re not alone. Millions of people experience whiplash each year, and most recover with the right care. As a chiropractor who treats whiplash patients regularly, I understand how scary and confusing these injuries can be. The good news is that with prompt attention and proper treatment, whiplash can heal, and you can get back to feeling like yourself again.
In this comprehensive guide, I’ll explain everything you need to know about whiplash in plain language – what it is, common symptoms to watch for, how long recovery might take, and what treatments actually help. My goal is to share both the medical facts and my firsthand experience in treating whiplash injuries, so you feel informed and reassured. Let’s start with the basics.
What Is Whiplash?
Whiplash is a neck injury caused by forceful, rapid back-and-forth motion of the neck, similar to the cracking of a whip. Essentially, the head is thrown in one direction and then snaps in the opposite direction. This sudden movement can strain or sprain the cervical spine (neck region), affecting muscles, tendons, ligaments, discs, and even nerves in the neck . Whiplash is often referred to as a neck sprain or strain, but it’s specifically associated with an acceleration-deceleration mechanism of injury. In other words, while a “neck strain” might also describe pain from sleeping awkwardly or a minor muscle pull, whiplash usually implies a more abrupt trauma where the neck was whipped beyond its normal range.
Common causes of whiplash: The leading cause is auto accidents – particularly rear-end car collisions. In a typical rear-end crash, your body is jolted forward while your head momentarily lags behind, then your head snaps forward and back. (Think of how a cracking whip moves – that’s what happens inside your neck.) But car crashes aren’t the only culprit. Whiplash can also result from other sudden impacts like contact sports injuries (for example, a football tackle or a hard fall in gymnastics), physical abuse or assault (being punched or violently shaken, as seen in shaken baby syndrome), or even falls where the head is whipped around.
It’s important to note that whiplash is an “invisible” injury – it doesn’t show up on a blood test and often not on X-rays either. It’s diagnosed based on symptoms and exam findings (more on that later). Even though you usually can’t see the damage on a scan, the pain and functional problems from whiplash are very real.
How whiplash differs from a general neck strain: In essence, whiplash is a type of neck strain/sprain, but it’s used to describe injuries from sudden trauma. A generic neck strain might come on from overuse or minor injury, usually affecting primarily the muscles. Whiplash, on the other hand, often involves a more complex injury mechanism, potentially affecting not just muscles but also ligaments, disks, and nerves due to the high forces involved . Whiplash injuries can lead to a wider range of symptoms (like dizziness or cognitive difficulties) compared to a simple stiff neck from sleeping wrong. In short, all whiplash is neck strain, but not all neck strains are whiplash. Whiplash tends to be more severe and is caused by an abrupt forceful motion.
What Are the Symptoms of Whiplash?
Whiplash can cause a constellation of symptoms, and they don’t always show up immediately. In fact, symptoms often start within 24 hours of the injury (sometimes not until the next day or two). It’s not uncommon to feel okay right after a minor accident, only to develop soreness later once your body has had time to stiffen up and inflammation sets in. Below are the most common whiplash symptoms to watch for:
- Neck Pain: This can range from a dull ache to sharp, stabbing pain in the neck. It often gets worse with movement – you might feel a jolt of pain when turning your head or looking up/down. The pain comes from strained muscles and ligaments, and sometimes joint irritation in the cervical spine.
- Neck Stiffness and Reduced Range of Motion: You may find your neck doesn’t turn or bend as far as it normally does. Muscle tightness and spasm can make it hard to move your head. Checking your blind spot while driving, for example, may be difficult due to stiffness.
- Headaches: Many people get headaches that start at the base of the skull and radiate up into the head. These are often called cervicogenic headaches, meaning they originate from neck injury. The headache may be constant or triggered by certain neck movements.
- Shoulder and Upper Back Pain: Whiplash doesn’t just affect the neck. You might feel soreness in your shoulders, between the shoulder blades, or in the upper back. The force can strain those areas as well, since the whole spine is involved in the whiplash motion.
- Dizziness or Vertigo: Some whiplash sufferers feel unsteady on their feet or dizzy. This could be due to neck injury affecting balance (cervical vertigo) or even a mild concussion if the brain was jolted. You might notice feeling lightheaded when you move your head quickly.
- Tingling or Numbness in the Arms or Hands: If nerves in the neck get irritated or pinched, it can cause radiating symptoms into your arm or hand. You might experience a “pins and needles” tingling sensation or numb patches in your fingers or arms. This is a sign the injury may be affecting nerve roots.
- Fatigue: It’s common to feel very tired or fatigued after a whiplash injury. Your body is recovering from trauma, and pain itself is exhausting. Sleep disturbances (see below) can also contribute to daytime fatigue.
- Difficulty Concentrating or Memory Problems: Some people describe “brain fog,” trouble focusing, or forgetfulness after whiplash. This can be part of whiplash-associated disorder, possibly related to concussion or just the stress of the injury. It should be temporary, but it’s certainly frustrating while it lasts.
- Irritability or Mood Changes: Being in pain can make anyone cranky. Beyond that, whiplash can sometimes influence mood directly, leading to unusual irritability, anxiety, or depressed feelings. These symptoms are part of the neurological/psychological aspect of whiplash-associated disorders for some patients.
- Ringing in the Ears (Tinnitus) or Blurred Vision: In some cases, people report ringing in their ears or vision disturbances. These are less common, but they can occur, especially if there was a concussion component to the injury.
Each person’s experience with whiplash is a bit different – you might have all of these symptoms, or just a few. It’s also important to note that symptoms can be delayed. You might feel fine right after the accident due to adrenaline, only to notice stiffness and headaches a day or two later. Delayed onset doesn’t necessarily mean the injury is more serious, but it does catch people off guard. I’ve had many patients exclaim, “I didn’t feel hurt at all at the scene – then two days later my neck was on fire and I started getting headaches.” This delay is exactly why I and other clinicians advise getting checked after a car accident even if you feel okay initially.
If you suspect whiplash from any kind of accident or injury, pay attention to these symptoms. Even mild pain is worth taking seriously, because prompt treatment can prevent things from getting worse.
How Long Do Whiplash Symptoms Last?
Whiplash symptoms typically last a few days to a few weeks, especially with proper care. Most people with mild to moderate whiplash (often classified as lower-grade whiplash) start feeling significantly better within 2–3 weeks . However, in more severe cases – especially if left untreated or if the injury is not managed properly – symptoms can persist for months or even become chronic .
In my clinical experience, the recovery timeline for whiplash varies widely. Here’s a general breakdown:
- Acute Whiplash (the first few days/weeks): Pain, stiffness, and other symptoms are usually worst in the first 24-48 hours after they begin, then gradually improve over the next several days. With early intervention (like gentle movement, therapy, etc.), many patients see steady progress. Most people feel considerably better within a month after a straightforward whiplash injury.
- Subacute (several weeks to a couple of months): For some, symptoms can linger 4-8 weeks. Typically by 6-8 weeks, the majority of whiplash injuries should be well on their way to healing. If you’re still having a lot of neck pain or headaches a few months out, that’s a signal to re-evaluate or try additional treatments.
- Chronic Whiplash: Unfortunately, a subset of people will continue to have pain and restrictions beyond the 3-month mark. “Chronic whiplash” or Whiplash-Associated Disorder chronic phase can include ongoing neck pain, stiffness, headaches, and other symptoms that last many months or even years . This is not common for mild cases, but it can happen, especially in more severe injuries.
Risk factors for a longer recovery (or developing chronic pain) have been identified. You may be more likely to have prolonged symptoms if:
- Your initial symptoms were intense and started very soon after the injury (for example, severe neck pain right at the scene of the accident). Rapid onset of pain can indicate a higher degree of tissue damage.
- You had limited neck mobility (very stiff neck) and pain radiating to the arms initially. These signs (which correspond to higher WAD grades) correlate with worse outcomes in studies.
- You are an older adult. Older individuals may heal more slowly due to less flexible tissues and may have pre-existing degeneration that complicates recovery.
- You’ve had whiplash before or already had neck/back pain prior. A history of neck problems can predispose you to slower recovery the next time around.
- The accident was high-impact or high-speed. More force generally means more severe injury. (That said, remember even low-speed crashes can cause whiplash; high speed just ups the odds of a bad sprain or other injuries like concussion.)
- Female gender may be a factor in some cases – research has shown women can be at higher risk for whiplash injuries and possibly longer-lasting symptoms, potentially due to differences in neck muscle strength and other anatomical factors.
- Not getting treatment early. Delaying care can increase the chance of chronic issues. If you just “tough it out” hoping it will go away, you might develop more scar tissue, muscle weakness from disuse, and even pain sensitization over time. Early diagnosis and intervention are key to a faster recovery.
To emphasize that last point: early active treatment helps whiplash heal. Traditional advice decades ago was to rest and wear a stiff collar for weeks, but we now know that approach can actually slow recovery . Movement is medicine for whiplash. One landmark study found that patients who started gentle neck exercises and movement shortly after the injury recovered faster and had less pain long-term than those who rested in a collar for an extended period . In my practice, I’ve seen that patients who begin treatment (chiropractic, physical therapy, etc.) within the first week or two tend to do much better at the 1-2 month mark than those who wait until pain has been around for a while.
Bottom line: Minor whiplash injuries usually resolve in a matter of weeks. More significant whiplash can take a couple of months. And without proper care – or if you have certain risk factors – whiplash can drag on and become a chronic source of pain. That’s why it’s so important to take it seriously and seek treatment early.
Whiplash from Car Accidents
Car accidents are by far the most common cause of whiplash. Even a seemingly “small” fender-bender can result in whiplash injury. Why are auto collisions so likely to cause whiplash? It comes down to the physics of a crash. When you’re in a moving vehicle that suddenly stops (or is struck from behind), your body is held in place by the seatbelt, but your head is not. The head keeps moving – and then snaps back – because of inertia. This rapid acceleration-deceleration force on the neck is exactly what causes whiplash.
To visualize it, imagine someone pulling a rug out from under you: your feet would fly forward but your head would whip backward. In a rear-end car accident, the seatback pushes your torso forward suddenly while your head lags behind, then your head is thrown forward. This can happen in a fraction of a second. The neck undergoes an abnormal S-shaped motion and extreme stresses beyond its normal range . It’s no surprise that the soft tissues can be injured in this process.
Even low-speed crashes can cause whiplash. Many people are surprised by this, but studies and crash tests have shown whiplash injuries at speeds as low as 5–10 mph. You don’t need a dramatic wreck to get a serious neck sprain. Factors like the angle of impact, headrest position, and the person’s own body can influence the outcome. I’ve seen patients with intense whiplash symptoms from a parking-lot tap, and conversely some walk away from a high-speed crash with little neck pain. So never assume you’re “fine” just because the crash was minor or your car has little damage.
The danger of ignoring symptoms after a crash: If you’ve been in an auto accident, it’s wise to get checked out even if you feel okay initially. Adrenaline and shock can mask pain in the moment. As noted earlier, whiplash symptoms might not surface until hours or days later. Don’t brush off even mild neck stiffness or headache after a collision – these can be early signs of whiplash. The danger in ignoring such symptoms is that you might have an injury that, left untreated, could worsen. For example, untreated whiplash can lead to chronic neck pain or prolonged dizziness that becomes harder to resolve. There’s also a small chance a more serious injury (like a cervical spine fracture or concussion) could be missed if you never get evaluated. Even low-speed impacts deserve medical attention to rule out anything serious and to manage whiplash properly.
In short, car accidents and whiplash go hand-in-hand. Always wear your seatbelt and ensure your headrest is properly positioned to reduce risk. Seatbelts and head restraints do help – they greatly reduce severe injuries and can mitigate whiplash severity by preventing extreme head movement. But they can’t always prevent it entirely. So if you’re in a collision and your neck “snaps” or you develop pain afterward, take it seriously. It’s better to be safe with an evaluation than to tough it out and end up with chronic issues.
(As a chiropractor in a region with plenty of drivers, I can’t stress this enough: some of the worst chronic neck cases I see started as “I thought it was just a minor fender-bender and didn’t get checked.”)
How Is Whiplash Diagnosed?
Diagnosing whiplash usually starts with a thorough history and physical examination. There’s no single lab test for whiplash, and as mentioned earlier, it often won’t show up on imaging scans. A healthcare provider – whether in the ER, your primary doctor, or a chiropractor like myself – will rely on what you tell them and what we find on exam.
Here’s what a typical whiplash evaluation involves:
- Medical History: We’ll ask about the incident (e.g. how the car was hit, your position, did you have immediate pain or not). Details of the crash or injury help gauge the force involved. We also ask about your symptoms – where it hurts, what movements make it worse, any tingling or headaches, etc. Don’t be surprised if we ask you to rate your pain or describe how it limits your daily activities; this helps us understand the impact on your function. We’ll also review prior injuries or conditions (for instance, if you already had neck arthritis, that could affect the diagnosis and treatment plan).
- Physical Examination: I will carefully palpate (feel) and move your neck, and also check areas like your shoulders and upper back. Key things we assess include:
- Range of motion: how far you can turn or tilt your head in each direction and where pain kicks in.
- Areas of tenderness: we press along the neck and shoulder muscles and joints to find trigger points or particularly sore spots.
- Muscle spasm or tightness: often, after whiplash, the neck muscles go into protective spasm.
- Neurological exam: This is important to ensure no nerve damage. We test your reflexes, arm and hand strength, and check for any numbness or tingling in your limbs. If certain reflexes are diminished or strength is reduced, it could mean a nerve root is compressed or irritated (which might bump the classification to a higher WAD grade, explained below).
- Overall function: We might ask you to perform simple tasks or movements that mimic daily activities to see what you can or can’t do without pain. For example, can you look over your shoulder, or how does it feel to raise your arms?
- Imaging Tests (if needed): While whiplash itself doesn’t have a definitive “spot” on an X-ray, imaging is useful to rule out other injuries. A standard X-ray of the neck may be ordered, especially if you had a hard impact, to check for fractures or dislocations. X-rays can also reveal degenerative changes (like arthritis) that might influence your recovery. If you have signs of possible disc injury or nerve compression (like arm numbness), or if severe pain continues, a CT scan or MRI might be recommended. MRI is particularly good at showing soft tissue – it can reveal bulging or herniated discs, ligament tears, or spinal cord impingement. The key point is, imaging is used to look for more serious issues that could cause similar symptoms (for example, a herniated disc) or complications, rather than to “see” a whiplash. Often, if initial X-rays are normal and there are no neurological red flags, advanced imaging is not immediately needed. (In practice, many whiplash cases won’t need an MRI unless symptoms don’t improve or there are unusual findings.)
- WAD Classification: Whiplash injuries are often categorized using the Whiplash-Associated Disorders (WAD) grading system, established by the Quebec Task Force. It’s a 0–4 scale used to describe the severity of whiplash:
- Grade 0: No neck pain or physical signs (essentially no injury).
- Grade I: Neck complaints of pain, stiffness, or tenderness, but no physical signs on exam. (This would be a mild whiplash where exam is pretty normal aside from your reported symptoms.)
- Grade II: Neck pain and musculoskeletal signs – such as decreased range of motion or point tenderness on exam. Most whiplash patients I see fall into this category: you hurt and we can objectively see that your neck is limited or tender.
- Grade III: Neck pain plus neurological signs – meaning exam finds nerve involvement like weakness, numbness, or reduced reflexes in the arms. This suggests a more significant sprain possibly affecting nerve roots.
- Grade IV: Neck pain with fracture or dislocation. (This is beyond a standard “whiplash” and into serious injury territory – typically managed in the emergency room.)
Using the WAD classification helps providers document the injury severity and decide on treatment. Generally, the higher the grade, the more intensive or prolonged the treatment might be. It’s also a prognostic tool – higher WAD grades tend to have longer recovery times. For example, someone with a Grade II or III injury might need a few months of therapy, whereas Grade I could resolve in a couple of weeks.
- Chiropractor’s role in assessment: As a chiropractor, I focus on the functional aspects of your neck injury. In addition to the above, I might do orthopedic tests (specific guided movements to pinpoint which tissues are affected) and assess your spine as a whole. Often we find joint restrictions in the neck or upper back from the whiplash, which we note for potential chiropractic adjustment. I also pay attention to posture and muscle imbalances. Importantly, I document all findings carefully – range of motion measurements, neurological exam results, pain levels – because this documentation not only guides treatment but can be crucial if this is a personal injury case (more on that later).
In summary, diagnosing whiplash is mostly about a good physical exam and patient history. If you ever have neck pain after trauma, expect your provider to poke and prod a bit and ask a lot of questions. They’re building a picture of which structures might be hurt. And if anything doesn’t fit the typical whiplash pattern – say, weakness in an arm or severe symptoms – they’ll use imaging or referrals to rule out more serious conditions.
Treatment Options for Whiplash Injuries
Treating whiplash usually requires a combination of approaches. The goals of treatment are simple: control pain, restore normal function/motion, and support the body’s healing process. As a chiropractor, I also emphasize preventing chronic issues by addressing the injury promptly. Here are the main treatment options and recommendations for whiplash:
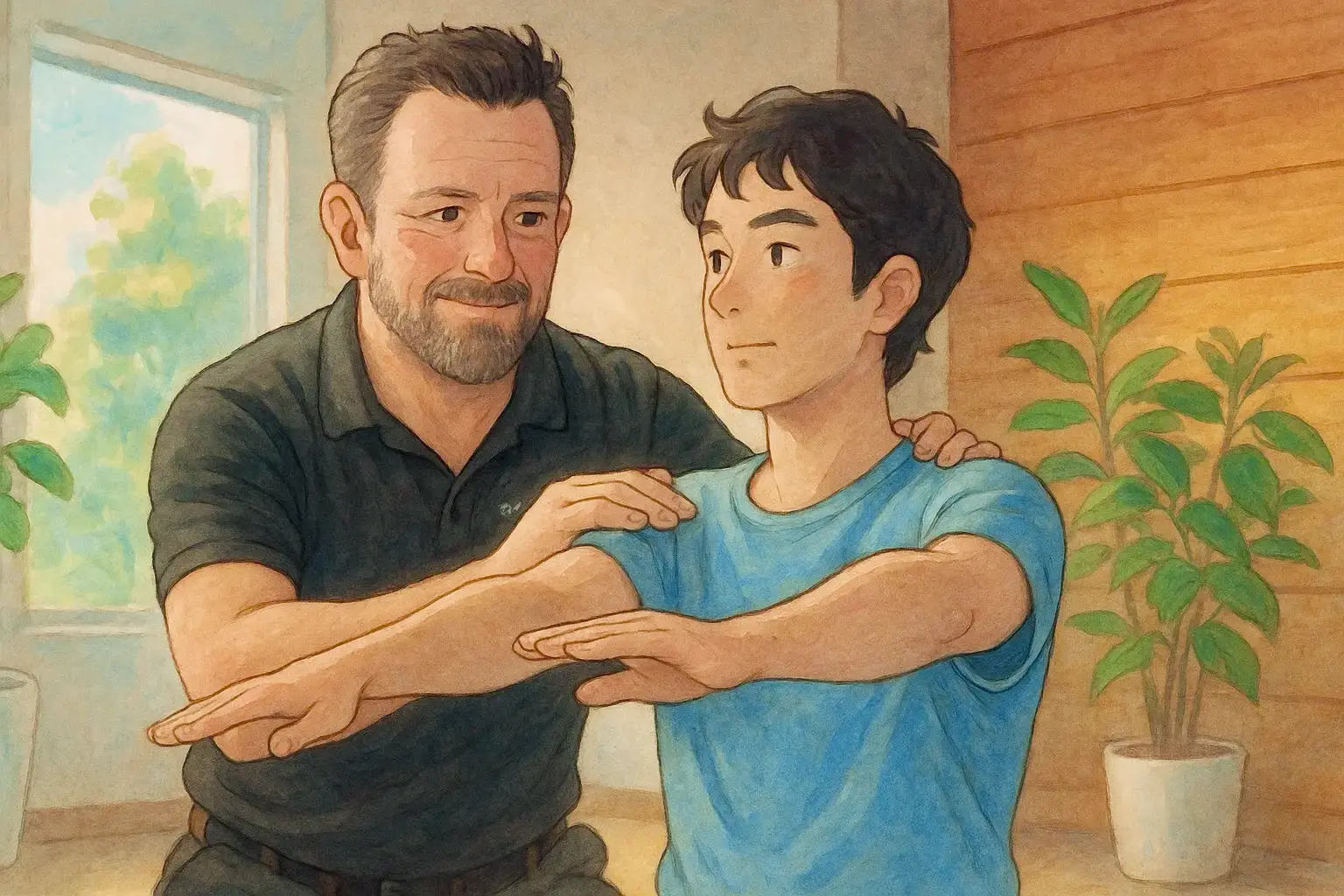
- Chiropractic Care (Spinal Adjustments): Chiropractic adjustments are a core treatment for many whiplash injuries. By gently manipulating the spine, we aim to improve joint mobility, realign any misalignments (subluxations) caused by the impact, and relieve pressure on irritated nerves. Many patients experience pain relief and better range of motion after a series of adjustments. In fact, some studies suggest chiropractic care can ease whiplash pain, especially when combined with exercise or physical therapy. In the acute stage, I use very gentle techniques – sometimes instrument-assisted or low-force adjustments – since the neck may be very tender. As you improve, more standard chiropractic manipulations can help restore normal motion in the neck. Chiropractic care also often includes other therapies like stretching, muscle release techniques, and home exercise guidance, making it a comprehensive approach. (Of course, I’m a bit biased, but I’ve seen countless whiplash patients recover faster with chiropractic in our clinic.)
- Physical Therapy: Formal physical therapy or therapeutic exercises are extremely beneficial for whiplash. A physical therapist can guide you through stretching and strengthening exercises to rehabilitate your neck and upper back. Early on, the focus is on gentle range-of-motion exercises – slowly rotating your neck, tilting side to side, and bending forward/back. Over time, as pain allows, therapy will include exercises to strengthen the neck muscles and improve posture (for example, using resistance bands or isometric exercises). PTs also use modalities like TENS (transcutaneous electrical nerve stimulation) – a mild electrical current that can reduce pain temporarily – or ultrasound therapy to help with tissue healing. The evidence shows that staying active and doing prescribed exercises speeds up recovery and prevents long-term stiffness . In practice, I often co-manage whiplash patients with physical therapists: chiropractic addresses the joint alignment and nerve aspect, while PT addresses muscle reconditioning. It’s a great combo.
- Therapeutic Massage and Soft Tissue Work: Whiplash almost always involves soft tissue strain. Therapists or chiropractors may perform massage therapy, myofascial release, or trigger point therapy to loosen tight neck and shoulder muscles. This can relieve pain and improve circulation to the injured area. Patients often report significant short-term relief from massage in the early weeks of whiplash. Even gentle techniques like craniosacral therapy or instrument-assisted soft tissue mobilization can help reduce muscle spasm and scar tissue formation.
- Ice and Heat: In the first 24-48 hours after injury, ice is recommended to reduce swelling and inflammation . Applying a cold pack to the neck for about 15 minutes at a time (with a thin cloth to protect the skin) a few times a day can numb pain and limit inflammation. After the initial acute phase, heat therapy often provides relief. A warm compress or heating pad for 15 minutes can relax tight muscles and increase blood flow to the area, which aids healing. Many of my patients find alternating heat and cold to be helpful: ice to calm acute pain, heat before doing stretching exercises. Just be cautious with heat right after the injury (stick to ice early on).
- Rest… but not too much: It’s okay to rest for the first couple of days when the pain is very fresh – your body needs time to recover. But prolonged bed rest or immobilization is not advised for whiplash. Studies have shown that more than a day or two of strict rest can actually slow recovery, leading to weaker muscles and stiffer joints . “Resting for more than a few days can cause the muscles in your neck, shoulders and back to get stiff and weak — and actually prolong the pain,” as one neurosurgeon puts it. So we encourage early, gentle movement within your tolerance. This might mean simply doing slow neck rotations at home or light activities. I often reassure patients: moving won’t damage your neck as long as it’s within a comfortable range – in fact, movement is exactly what your neck needs to heal.
- Pain Medication (as needed): Medication can help manage symptoms, though it’s usually not a standalone treatment for whiplash. Over-the-counter pain relievers like acetaminophen (Tylenol) or NSAIDs (e.g. ibuprofen) are commonly used to reduce pain and inflammation. These can be quite effective for mild to moderate pain in the short term. If pain is more severe, a doctor may prescribe stronger medications. For example, muscle relaxantsmight be given for a week or two to calm muscle spasms. Sometimes a short course of prescription NSAIDs or even certain nerve pain medications (like a low-dose tricyclic antidepressant or gabapentin) are used if there’s nerve-related pain. We use medications judiciously – the idea is to make you comfortable enough to participate in therapy and stay active. Long-term use of pain meds or opioids is generally not recommended for whiplash; the focus should be on active rehab.
- Injections: In a few cases, if a particular muscle or facet joint in the neck is a persistent source of pain, a medical doctor might perform a trigger point injection or facet joint injection with a local anesthetic. The Mayo Clinic notes that a numbing injection (like lidocaine) into painful muscle areas can decrease pain enough to allow better participation in physical therapy. These injections are usually considered if other treatments aren’t providing enough relief, and they tend to be a short-term aid.
- Cervical Collar (Brace): You’ve probably seen people after accidents wearing those foam neck collars. Soft cervical collars were once a mainstay of whiplash treatment, meant to immobilize the neck and provide support. Now, we use them sparingly. Why? Because keeping the neck completely still for too long can lead to weaker muscles and slower recovery. That said, a collar can be useful in the very acute phase or for short periods. For example, if it’s very painful to hold your head up initially, a soft brace for a day or two or wearing it at night might help. Experts have differing guidelines – some say no more than 72 hours of use, others allow a few hours a day for a couple of weeks in certain cases. The current best practice is to minimize collar use and encourage motion, but use your provider’s guidance. I typically only recommend a neck collar if a patient is in so much pain they can’t function otherwise, and even then, just briefly.
- Home Exercises and Stretches: Beyond formal PT, doing prescribed exercises at home is crucial. Simple range-of-motion exercises like those mentioned earlier (gentle rotation, tilting, nodding “yes” and “no”) done several times a day help prevent stiffness. As you improve, we add isometric strengthening (pressing your head lightly into your hand in various directions) and postural exercises (like chin tucks to train the deep neck flexor muscles). I also advise patients on ergonomics – for instance, using a supportive pillow, avoiding cradling the phone on the shoulder, setting up a desk chair that supports the head and neck. Little changes can make a big difference when recovering from whiplash.
- Other Therapies: Some patients explore acupuncture, which may offer relief for neck pain in some cases. Acupuncture involves inserting fine needles in specific points and can reduce muscle tension and pain for some individuals. There’s also mind-body therapies like gentle yoga or tai chi – these focus on slow movements and breathing, which can help reduce pain and improve mobility over time. These are generally safe to try in conjunction with other treatments, as long as you stick to gentle versions appropriate for your condition.
In essence, whiplash treatment is a multidisciplinary effort: chiropractors, physical therapists, medical doctors, and sometimes massage therapists all play a role. As a chiropractor, I often act as a quarterback for the care, ensuring that the patient gets the adjustments, exercises, and any needed referrals for things like pain management. An important piece of the puzzle is also patient education – teaching you how to move correctly, how to do exercises, and what activities to avoid or modify while you heal.
One more note: early intervention cannot be overstated. Research has shown that getting moving and into therapy sooner yields better outcomes than waiting. A review of treatments concluded that early mobilization leads to improved pain and faster return to normal life, whereas prolonged rest or delayed treatment can hinder recovery . So if you’re sidelined with whiplash, don’t wait weeks hoping it magically disappears – start treatment as soon as you’re able.
When to Seek Help (And What Happens If You Don’t)
If you suspect you have whiplash (or any significant neck injury), you should seek medical evaluation promptly – ideally within a day or two of the injury. Sometimes people hesitate, thinking “It’s not that bad” or hoping it will just get better on its own. But here are some clear signals that you should see a healthcare provider:
- Severe or increasing neck pain: If your pain is intense, or if a moderate pain is worsening instead of improving after a couple days, get it checked. Severe pain could indicate a more serious injury (like a ligament tear, herniated disc, or even a fracture) that needs specific management.
- Pain radiating into shoulders or arms: Any numbness, tingling, or weakness in your arms or hands is a red flag for nerve involvement. This warrants prompt evaluation to prevent potential permanent nerve damage.
- Severe headache or changes in consciousness: A headache that is worsening or accompanied by difficulty concentrating, extreme drowsiness, or confusion could suggest a concussion or more severe neck injury. After a car accident, if you have a new severe headache or feel “foggy,” see a doctor.
- Dizziness or balance issues: While some dizziness can occur with whiplash, if you’re having trouble with balance or episodes of vertigo, it’s wise to get it assessed. There could be vestibular involvement or even a subtle brain injury.
- Difficulty swallowing or any trouble with speech/vision: These are less common, but if present, could indicate a serious injury like a higher cervical spine issue.
- No improvement after a week or two of home care: If you tried rest, over-the-counter meds, and maybe some basic stretches, but after a week you’re no better (or worse), it’s time for professional help. Whiplash pain that isn’t improving may need targeted therapies or could be something more complex than a simple strain.
Now, what happens if you don’t seek help and just ignore a whiplash injury? There are a few potential consequences:
- Chronic Pain: The most common risk of untreated whiplash is that pain becomes chronic. Instead of resolving in weeks, the pain can linger for months or even years . Chronic neck pain can be debilitating – it may lead to dependency on pain medications, difficulty with daily activities, and a decrease in quality of life. Studies have shown that a significant fraction of whiplash patients report some level of symptoms years later, especially if initial injuries were not addressed.
- Lasting Stiffness and Reduced Mobility: Without proper rehab, the neck can heal in a tightened, less mobile state. Scar tissue forms as the strains heal, and if you haven’t been working on flexibility, you could be left with a permanently reduced range of motion. I’ve seen patients who can barely turn their head months after an accident because they never exercised or got treatment – their muscles essentially “froze up.” This kind of lingering stiffness can also predispose you to further injuries.
- Muscle Weakness and Compensation Injuries: If it hurts to move your neck, you might start moving differently to avoid pain (for example, twisting your entire body instead of your neck). Over time, this can weaken the neck muscles and strain other areas. Untreated whiplash can lead to chronic muscle imbalances – weak deep neck flexors, tight upper back muscles – which in turn can cause tension headaches or mid-back pain down the road.
- Neurological Issues: In certain cases, what seems like a simple whiplash could actually involve a herniated disc in the neck compressing a nerve. If that goes untreated, you could have persistent arm pain, numbness, or even long-term nerve damage. There’s also a rare but dangerous condition where instability in the cervical vertebrae can injure the spinal cord – missing that because one didn’t get checked could be catastrophic (though I stress, this is rare and usually would have severe initial symptoms).
- Worsening of Symptoms: Some whiplash-associated symptoms like dizziness, headaches, or jaw pain (TMJ issues can arise from the jolt) might start off minor but get worse without treatment. For instance, that dull headache could turn into chronic migraines triggered by neck tension if not managed.
- Psychological Effects: Living with untreated chronic pain can lead to anxiety, depression, or sleep disturbances. Whiplash patients with long-term pain often report poor sleep (neck pain makes it hard to get comfortable) and that can spiral into fatigue and mood changes.
The key takeaway is that prompt care leads to faster and more complete recovery. One article put it succinctly: the sooner you address whiplash, the more you can do to alleviate pain and prevent the injury from worsening. From a clinician’s perspective, it’s easier to treat a fresh injury than one that’s become chronic and complicated by months of adaptive changes. Early intervention can break the pain cycle before it sets in.
If you ever have a whiplash injury, don’t “tough it out” for too long. A quick check-up can rule out serious issues and set you on the right course. And if you decide not to seek care and things aren’t improving, please reconsider – your future self will thank you for taking care of it before it becomes a constant problem.
(As a side note, seeking prompt medical attention also documents your injury early, which is important if the accident leads to a personal injury claim. More on that next.)
Whiplash and Personal Injury Claims
Whiplash injuries are not only a health concern – they often become a legal/insurance concern, especially when they result from car accidents. If your whiplash happened in a motor vehicle collision that was someone else’s fault, you may be involved in a personal injury claim. In these cases, accurate documentation and consistent treatment are critical.
Why does documentation matter? In personal injury claims (like an auto insurance claim or lawsuit), you need to prove that you were injured and show the extent of your injuries. Whiplash is sometimes met with skepticism by insurance companies because it’s a soft tissue injury (you can’t “see” it on an X-ray). This is where your healthcare provider’s records become key evidence. As a chiropractor experienced in personal injury cases, I make sure to chart everything: your initial pain levels, exam findings (like limited range of motion, muscle spasm, neurological signs), the diagnosis (e.g. WAD Grade II cervical sprain/strain), and all treatments provided.
Chiropractors play a vital role in documenting whiplash injuries. We are licensed healthcare professionals, and our documentation is just as valid as an MD’s when filing an injury claim. In fact, chiropractors often see whiplash patients early and frequently, so we compile detailed notes on how the injury progresses over time. This can include daily or weekly progress reports, which are very helpful in showing an insurer or attorney how the injury has impacted you. We note improvements, setbacks, and any activities you still struggle with (for example, if a month after the accident you still can’t lift your child due to neck pain, that goes into the record).
Good documentation typically includes: the initial assessment and diagnosis, the treatment plan, and ongoing progress notes showing how you responded to treatment. It should also record things like referrals for MRI or to specialists if needed. All of this builds a picture that your injury was real, was caused by the accident, and required a certain amount of care to recover.
From a legal perspective, consistent treatment following the injury is often taken as evidence that you were indeed hurt and actively trying to get better. Large gaps in care or not following through with recommended therapy can hurt a personal injury case – the opposition might argue that your injuries weren’t serious or that you failed to mitigate (reduce) your damages. So, if you have a claim, it’s important for both your health and your case to attend all doctor/chiropractor appointments and follow the care plan.
Additionally, a chiropractor or other provider may be asked to provide a final report or narrative for the personal injury case, summarizing your injuries, treatment, and any residual deficits. We might also assign an impairment rating if you have any permanent limitations. I’ve worked closely with many personal injury attorneys who value a well-documented file; it helps in negotiating settlements when we can clearly show the before-and-after difference in a patient’s condition.
In summary, if you’re dealing with whiplash as part of a personal injury claim:
- Get evaluated and start treatment as soon as possible. Not only for your well-being, but early medical records linking the injury to the accident are crucial.
- Ensure all your symptoms are noted – even things that seem minor (like slight dizziness or trouble sleeping) should be recorded, because they paint a full picture of your post-accident condition.
- Follow through with care and keep your appointments. It demonstrates that you’re doing your part to recover.
- Keep your own notes if needed about how the injury affects your daily life (many attorneys like clients to keep a pain journal). You can share these with your provider so they are included in the medical record.
- Know that chiropractic documentation is absolutely recognized in injury claims. Chiropractors are experts in musculoskeletal injuries from car accidents and can accurately diagnose and document the full extent of whiplash injuries. This documentation is crucial for your insurance claim and any settlement negotiations.
One more thing: while it’s beyond the scope of this article to delve deep into legal advice, be cautious about insurance adjusters who downplay whiplash. It’s a real injury – the medical literature supports it – and with proper documentation from your providers, you have the evidence on your side.
Conclusion: Healing Whiplash the Right Way
Healing from a whiplash injury requires a mix of patience, proper treatment, and self-care. The aftermath of a car accident or any injury can be overwhelming – you’re in pain, maybe dealing with insurance, and just trying to get through your day with a stiff neck. I want to assure you from my experience: with early intervention and a good rehab plan, the vast majority of whiplash patients get back to 100% or very close to it. Neck tissues do heal. Pain does subside.
A few parting pieces of advice on the road to recovery:
- Listen to your body – gentle movement is good, but don’t push into sharp pain. There’s a difference between therapeutic exercise discomfort and harmful pain. Your provider will help you learn that line.
- Stay engaged in your treatment – whether it’s chiropractic visits, physical therapy sessions, or home exercises, consistency is key. Each little exercise or adjustment is a building block in your healing.
- Take care of your whole self – icing after a long day, using a supportive pillow at night, keeping good posture at your workstation, managing stress (stress can amplify pain) – it all matters. Whiplash is a holistic injury, and it recovers best with a holistic mindset.
- Don’t get discouraged if you have a setback. It’s normal to have good and bad days. The trajectory is usually two steps forward, one step back – but over time, those steps forward win out.
Most importantly, don’t ignore what your body is telling you. Pain or other symptoms are signals that something needs attention. If you or someone you care about has symptoms of whiplash, early assessment is critical. It can rule out serious issues and get you on a treatment track before chronic problems develop.
As a chiropractor, nothing makes me happier than seeing a whiplash patient regain their quality of life – being able to turn their head without pain, sleep through the night, and resume all the activities they love. It’s absolutely possible with the right approach to healing.
If you’re in the Petaluma area (Sonoma County, CA) and need a professional evaluation or treatment for whiplash, reach out to us at adjust.clinic – we’re here to help. You’re not alone on this healing journey. With expert care and a bit of time, you can put whiplash in the rearview mirror and move forward feeling your best.
Frequently Asked Questions (FAQs)
Q: Can whiplash symptoms be delayed even if I felt fine right after the accident?
A: Yes. It’s very common for whiplash symptoms to be delayed by 24-48 hours (or more) after an accident. In the immediate aftermath of a crash, your adrenaline is high and you might not feel pain due to shock. Many people start noticing neck stiffness, headaches, or other symptoms the next day or even two to three days later. Just because symptoms were delayed doesn’t mean the injury is “minor” – it’s still whiplash, and you should address it. This is why it’s wise to get checked by a doctor or chiropractor after an accident, even if you feel okay at first. Early documentation of any soreness or limited motion can also help in case symptoms worsen later.
Q: How is whiplash different from a regular neck strain or sprain?
A: Whiplash is essentially a type of neck sprain/strain caused specifically by a sudden acceleration-deceleration force (like in a car accident). A regular neck strain might occur from something like poor posture or lifting something heavy and typically involves just the muscles or tendons. Whiplash, by contrast, often involves a rapid, extreme motion that can injure multiple structures in the neck at once – muscles, ligaments (sprain), disks, and nerves. It also frequently comes with additional symptoms like dizziness or cognitive fog that you wouldn’t usually get from a simple muscle strain. In short, whiplash is a more complex injury mechanism. It’s a neck strain/sprain plus a biomechanical trauma component. Clinically, we treat whiplash in a more comprehensive way because of these potential additional issues, whereas a common neck strain from sleeping wrong might just need a few days of rest and heat.
Q: Do I need to wear a neck brace (cervical collar) for whiplash?
A: In most cases, no, you won’t need a cervical collar or you’ll only use one briefly. The old-school approach of keeping the neck immobile in a brace for weeks has fallen out of favor. We’ve learned that prolonged immobilization can lead to muscle weakening and actually slow recovery. Instead, we encourage gentle movement. That said, a soft neck collar can be useful in the first few days if your pain is severe – for example, wearing it for short periods to support your neck during travel or sleep. But you should not depend on it long-term. Generally, if a collar is used, it’s only for a day or two continuously, or a few hours a day for a couple of weeks at most. Your healthcare provider will guide you. Many patients don’t use a brace at all. The focus will be on therapies and exercises to strengthen and restore your neck function, rather than keeping it still.
Q: What’s the fastest way to recover from whiplash?
A: The “fastest” way is to start treatment early and stay consistent with it. That means:
- Get evaluated as soon as possible so that you can catch any issues early and start a rehab program.
- Use ice in the first 1-2 days, then transition to gentle heat and movement as advised.
- Follow your chiropractor or physical therapist’s exercise recommendations – doing your home stretches/exercises daily can speed up healing.
- Keep moving in moderation; avoid heavy lifting or strenuous activity that aggravates pain, but don’t keep your neck totally still. Simple activities like short walks (if safe) or easy range-of-motion movements help circulation and healing.
- Stay ahead of pain: use prescribed medications or anti-inflammatories judiciously to manage pain enough that you can move and sleep, since good sleep aids recovery.There’s no magic overnight cure, but patients who are proactive – attending all therapy sessions, doing their home exercises, and not delaying care – tend to recover notably faster. For instance, someone who starts therapy within a few days may recover in weeks, whereas delaying therapy a month could prolong recovery. Also, addressing the injury holistically (with physical treatment and attention to nutrition, hydration, and rest) will give your body the best conditions for rapid healing.
Q: Can a chiropractor really help with whiplash?
A: Absolutely, yes. Chiropractors specialize in musculoskeletal injuries like whiplash and are trained to treat spinal and soft tissue injuries from accidents. Chiropractic care can help restore proper alignment and mobility in the neck, which is often disrupted in whiplash. Adjustments can alleviate pain by reducing pressure on nerves and relaxing muscle tension. In addition, chiropractors often incorporate rehab exercises, stretches, and other therapies (like electric stimulation or ultrasound) as part of a whiplash treatment plan. We take a drug-free, movement-oriented approach that complements the body’s natural healing. Many patients find that chiropractic treatments significantly reduce pain and improve their range of motion after whiplash. It’s also worth noting that chiropractors provide comprehensive documentation of your injury and progress, which can be helpful if you have an insurance claim. Always ensure you see a licensed chiropractor with experience in whiplash/personal injury cases. In sum, chiropractic care is often one of the frontline treatments for whiplash and can be very effective, especially when combined with other therapies in a well-rounded recovery plan.